 Dr. Siddhartha Ghosh
Dr. Siddhartha Ghosh
Consultant Ophthalmologist (MBBS, MS)
In Diabetes Mellitus our body does not use or store sugar properly. This can cause permanent structural changes in the blood vessels of the retina of our eye and also in other organs of our body. This may affect our vision adversely. This is called Diabetic Retinopathy.
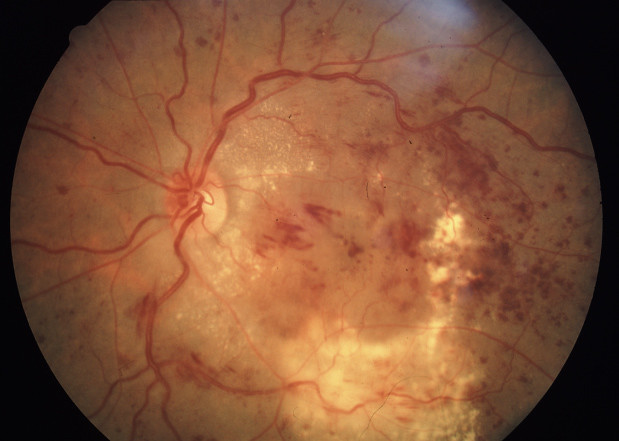
There are two types of Diabetic retinopathy. One type is called Non-Proliferative Diabetic Retinopathy (NPDR) and the other more advanced type is called Proliferative Diabetic Retinopathy (PDR).
In NPDR, damaged blood vessels in the retina begin to leak fluids including small amounts of blood in the retina. Sometimes deposits of fat may leak inside the retina; these exudates are called hard exudates.
With macular edema, blood leaking from the retina's blood vessels can cause the macula to thicken or swell. As macula is the centre of our precise or pinpoint vision, any swelling in the macula will therefore cause deterioration of central vision.
Macular ischemia occurs when small blood vessels close. Here again the macular function is affected as it does not receive enough blood supply required to maintain good vision.
During an eye examination, pupils are dilated with eye drops, so that the inner layer of the eye, which is the retina, is visible clinically. In addition, certain imaging studies of the retina like the fluorescein angiography (FFA) and the optical coherence tomography (OCT) may be recommended to gather more precise information about the damage caused by retinopathy and to plan treatment.
With PDR, many smaller blood vessels in the retina close, preventing adequate blood supply to the retina. The retina responds to this problem by trying to grow new vessels. These new blood vessels are however unable to maintain adequate blood supply to the retina and can spontaneously bleed or cause scar tissue formation. This may lead the retina to wrinkle or to detach. If similar vessels grow in front of the eye, they can block the drainage channel of the eye and can elevate the eye pressure thereby leading to a condition called neo-vascular glaucoma. So, both central and peripheral vision can be affected in PDR.
In many cases vision may be stabilized by laser treatment. Treatment with laser is performed in an out-patient department (OPD) setting. For comfort during the procedure, an anesthetic eye drop is applied. For macular edema the laser is focused on the retina, around the centre of the macula, and this is called focal laser photocoagulation. The main goal is to seal off the leaking blood vessels that interfere with the proper functioning of the macula. In PDR, laser is applied to the periphery of the retina, and this is called pan retinal photocoagulation (PRP). PRP leads to shrinkage of the existing new vessels and also prevents further formation of new vessels in the future. This may reduce chances of further bleeding in the retina and vitreous. When vitreous hemorrhage occurs, a surgical procedure called vitrectomy may be required to clear off the blood and scar tissue, and is often additionally treated with endo-laser to the peripheral retina.
However, it should be remembered that the main aim of treatment for diabetic retinopathy is to prevent further vision loss. Diabetic Retinopathy cannot be cured but total blindness is uncommon if treated early. Most people with diabetes can retain useful vision. A regular eye examination can help diagnose and treat Diabetic retinopathy early. Therefore a routine eye examination is mandatory in all diabetics, even if they don't have any vision problem. This may help preserve useful vision for a lifetime.